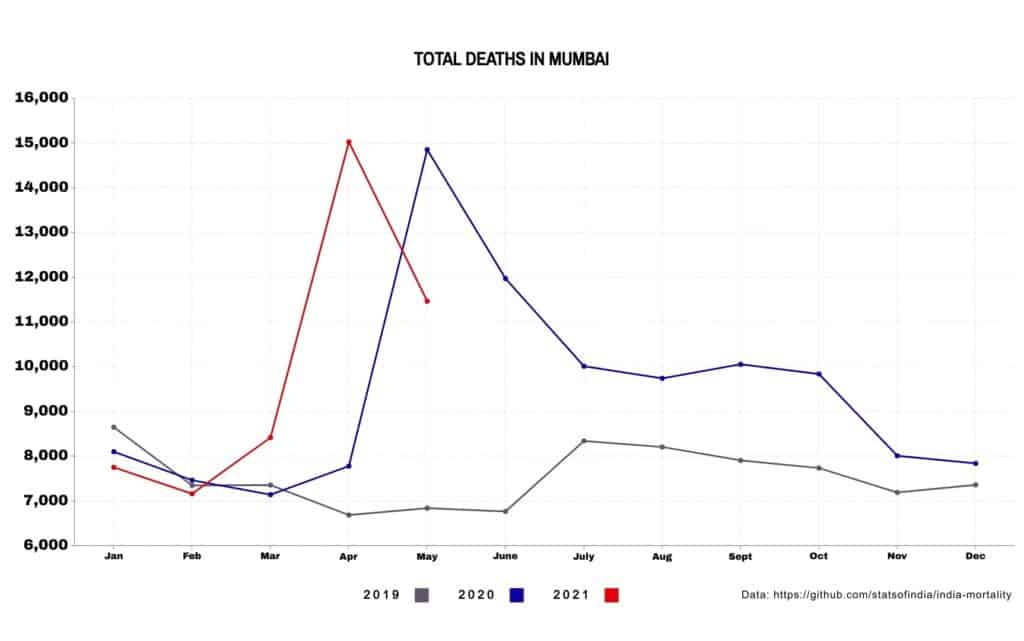
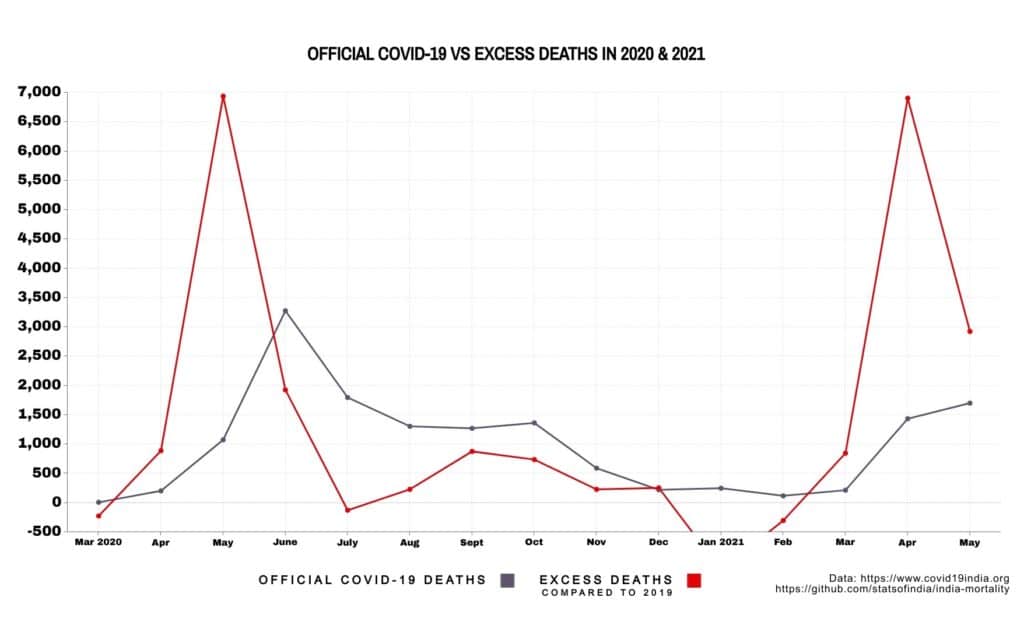
In May 2020, during the first wave of the COVID-19 pandemic, 14,857 people died in Mumbai. This was over twice the number of deaths that occurred in May of the previous year. Official COVID-19 deaths, however, accounted for barely 15% of them – 1,075 out of 8,014.
The number of deaths increased in comparison to 2019 till October 2020. Over the year, they added up to 20,719 more deaths over 2019’s toll, but only around half, 11,116, were officially due to COVID-19. The rest are unexplained.
A spike in the number of deaths was seen again with the second wave in April 2021, which witnessed 15,031 deaths – a 94% increase in comparison to deaths in April 2020. While 1,435 were official COVID-19 deaths, 5,840 were unexplained.
Were these ‘excess deaths’ undercounted, deliberate or otherwise, COVID-19 deaths? If not, what’s the explanation for them?
Investigation Pending
A stringent lockdown and an already overwhelmed healthcare system brought the country to its knees when the pandemic struck.
As a result of this, healthcare services for non-COVID-19 patients were also affected. In a COVID-19 impact survey done by Praja Foundation in December 2020, 33% of respondents admitted to facing difficulty in accessing healthcare for non-COVID-19 issues.
This was probably why registrations of major diseases (Tuberculosis, Diabetes, Malaria, Dengue, etc) showed a decline by 29% in 2020, as stated in Praja Foundation’s State of Health in Mumbai in 2021 report.
“You don’t get such a huge surge in deaths over a short period of time from other causes – this is very much the signature of an epidemic,” says Murad Banaji, a mathematician at Middlesex University, London. Murad and Aashish Gupta, a demographer, estimate excess deaths in India to range from 2.8 million to 5.2 million in a paper that is not peer reviewed as yet.
In multiple reports, officials from the COVID-19 death audit committee and BMC promised an investigation into the ‘excess deaths’. But according to the Assistant Health Officer in the Municipal Corporation of Greater Mumbai (MCGM), Dr Mangesh Kumbhare, no such investigation has been conducted.
“It’s possible that we have missed out on some deaths that did not test for COVID-19,” says Dr Pradip Awate, Maharashtra’s state surveillance officer. “But in Mumbai and Maharashtra, we have established COVID-19 death audit committees at every level, so we can’t have missed more than 5% of COVID-19 deaths.”
Read more: COVID-19 mitigation measures have led to the neglect of one of Mumbai’s top killers
Evidence of COVID undercounting
It is unmistakable, to Murad, that the unexplained high death numbers in early 2020 are due to COVID-19. In Mumbai particularly, data from serosurveys and journalists alongside official data have allowed a detailed picture of the spread of infections across wards. The culprit for the high undercount, he writes in a Scroll.in article, is underreporting from marginalised areas in the city.
His mapping reveals that the virus first attacked the slums: a serosurvey conducted in July 2020 revealed that 70% of the city’s infections were found in slums. But official case data from municipal wards of different slum populations did not mirror this, since under 1% of infections from slums had been captured during testing. The rapid spread of infections in slums was worsened by uneven detection and reporting.
The resulting Infection Fatality Rate (IFR) – the percentage of infections that translated into deaths – was also skewed. In the slums, it was around 0.076%, and in wealthy areas around 0.263%. Murad notes that a strain of wishful thinking dared suggest that slums, due to their younger population, got lucky. But the rise in ‘excess deaths’ earlier in 2020 indicates a different story.
After what Murad called a ‘slum surge,’ overall deaths reduced in the city and the COVID-19 death toll steadied. The undercount factor, the ratio of excess deaths to recorded COVID-19 deaths, went from 3 at the end of June 2020, to 1.5 between August 2020 and December 2020. By September 2020, the BMC said that 80% of new cases were being reported from non-slum areas, and hence a smaller number were going uncounted.
In contrast, the surge in infections during the second wave occurred in both slum and non-slum areas. “On-ground reports suggested that the slums were not affected to the same extent, in terms of mortality and hospitalisation, in 2021 as they were in 2020. But we need to be cautious, because we know that infections and deaths have a higher chance of getting missed in slums,” says Murad. The lack of ward-wise death data, however, masks how many of the infections translated into deaths.
“What I would like to know is where these deaths were occurring: most people have assumed they were mainly in non-slum areas, but if there were many excess deaths in the slums in 2021, that would change the story of Mumbai’s epidemic,” he says.
Missing ’cause of death’ data
In its annual health reports of the state of health in Mumbai, the Praja Foundation conducts a mortality analysis of deaths that occurred in the city. Using Cause of Death (COD) data acquired from the government, it compares the number of deaths due to different causes from year to year. This could give clues to the excess deaths. But in their 2021 report, the analysis for 2020 is absent.
The reason for this, says the report, is, “MCGM mentioned that they were in the process of collating the COD for 2020-21 hence it is yet to be completed.”
Access to this data has been a problem for the MCGM and State Government since 2016, when the central government made changes to the system for Registration of Births and Deaths. Information about deaths – including age, gender, date, cause and location – that was previously entered into the MCGM’s System Application Protocol (SAP) software was switched to being entered into the Civil Registration System (CRS) software, managed by the central government. This was done to maintain uniformity and increase registrations of births and deaths across the country.
“We have to access the data, analyse and then generate it, and only then can we provide it. It is not like a financial report that has to be submitted at the end of the year,” says Dr Mangesh Kumbhare.
On the RTI trail
Following established procedure, the Praja Foundation sent the MCGM an RTI request for COD data for the first quarter of 2016. They received a surprising reply: the MCGM did not have COD data due to a technical issue. “When reports were seen in CRS system, it is observed all the fields are showing zero figures,” said the RTI.
Neither did the state government’s Health Intelligence and Vital Statistics (HIVS) division, stated another RTI reply.
“There is a clear gap in the transition process,” says Yogesh Mishra, Research and Data Head at the Praja Foundation. “If the MCGM handed over registration to the central government, they should have questioned them about it. But they didn’t even notice their lack of access until we filed an RTI. How are they monitoring their health policies and forming the health budget without cause of death data?”
“The problem of access to CRS data is there all over India. We’ve written to the central and state government about the difficulty in generating all data about mortality, and they are working on it,” says Dr Mangesh Kumbhare.
It took another three years of multiple RTIs, letters, appeals and non-followance complaints to the central government’s Vital Statistics Division (VSD) and Central Information Commission (CIC) to receive data for 2016, 2017 and 2018. This was the result of a compilation by the MCGM, as the state and local governments were not given access to the CRS software. (A detailed timeline of the RTIs, letters and responses filed and received by Praja is documented in the annual health reports.)
“The evasion of providing this data in the public domain appears to be purposeful, in the face of the revealing status of health in the country that the cause of death data brings forth,” reads the report. This was partially rectified in mid-2020, when the state government was given access to CRS data for 5 corporations (MCGM, Nagpur, Nasik, Aurangabad and Pune).
COD data for 2019 was again delayed till 2021, and is still pending for 2020.
[Note: Slight fluctuations exist in death data depending on source. Data used here is from covid19india.org, India Mortality Dataset on Github (compiled and aggregated by Pratap Vardhan) and the MCGM Vital Statistics Report.]